X-ray Ventilator Synchronization
Reducing patient radiation exposure and speeding up the process for X-ray technicians
Context
- When
- 2010 – 2011
- My Role
- Engineer
Patients on ventilators receive excess radiation from their daily chest X-rays. And X-ray technicians have to manually capture good quality X-rays before an attending physician can do her morning rounds. For an average 12-patient room, the technician would spend over 3 hours to capture the optimal images.
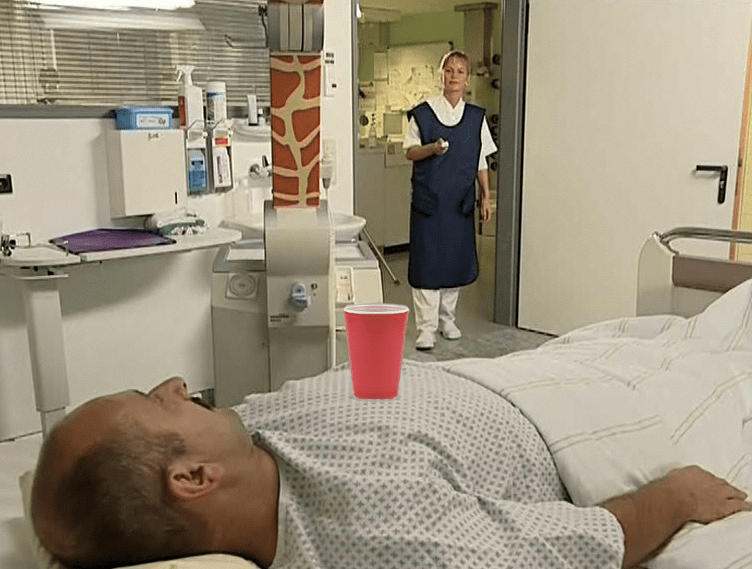
Some technicians created workarounds to speed up the process – including placing a plastic cup on the patient’s chest to better visualize the lung cycle from the room next door. Our solution automated X-ray capture and optimized the diagnostic value of the images.
Capturing optimal diagnostic images
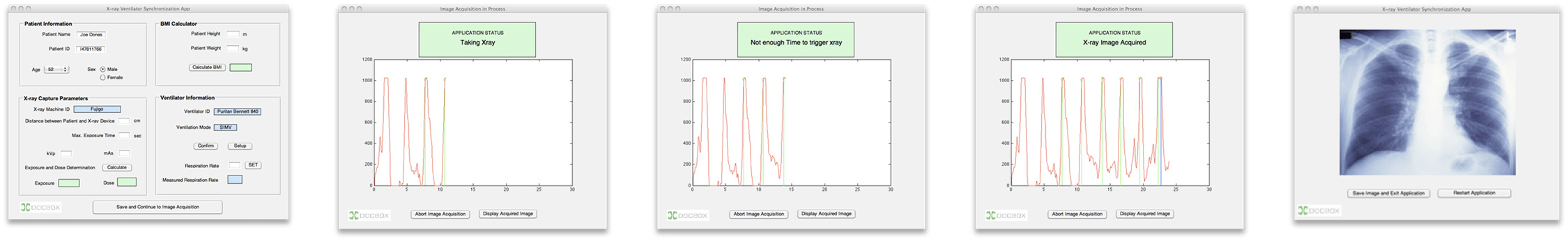
For my senior project at Boston University, I teamed up with two of my classmates, DocBox, and the Medical Device Plug-and-Play Lab of Partners HealthCare. We wanted to solve the image quality problem by using physiological data from the ventilator to:
- analyze the patient's phase of respiration
- predict when the patient will be at full inflation
- and automatically trigger the X-ray machine to capture an optimal diagnostic image

This had to be possible in two modes of ventilation:
- Assist/Control (A/C), where the ventilator triggers a breath for a patient at regular intervals
- Synchronized Intermittent Mandatory Ventilation (SIMV), where the ventilator triggers a breath for a patient only when the patient needs help with respiration

Predicting the point of full inflation
Predicting the exact moment when the patient is at full inflation is easier in A/C mode than in SIMV mode. In A/C mode, we could rely on the ventilator to bring the patient to the same lung pressure at full inflation in each breath. We could use the maximum pressure over three breaths to set a threshold. Then we'd capture an X-ray after the next time that threshold is met.

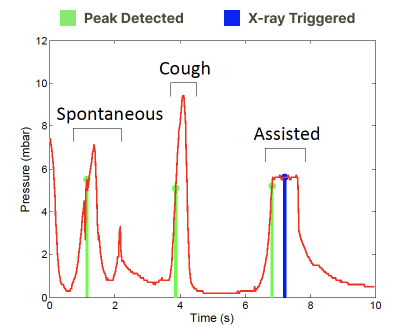
In SIMV mode, we could not rely on the same assumptions to predict the phase of respiration. I designed a state machine algorithm to help us differentiate an assisted breath (when we wanted to capture an X-ray), from a spontaneous breath or cough.

The state machine would continuously compare the last two lung pressure readings and determine if the pressure was rising, falling, or in free fall. To avoid capturing X-rays on a breath or cough, I added a low pass filter to smooth the waveform.
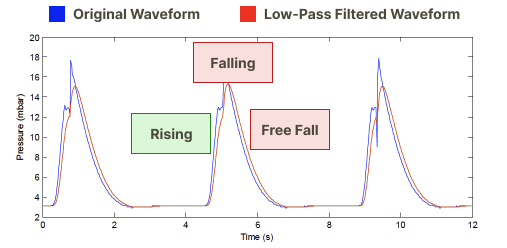
After adjusting the parameters of the filter, we were able to accurately predict the point of full inflation with 94% accuracy using 5 different data sets of patients on mechanical ventilators.
Comparing results to the manual method
Before handing off our project to our partners at DocBox for clinical trials, we analyzed the limitations of our algorithms and performed a hazard analysis of our system.
We provided the severity, probability, and mitigation strategies for each hazard (such as delays associated with trigger signaling and X-ray image capture or the patient coughing).
This allowed DocBox to proceed with clinical testing. Although we did not quantify the time saved by each technician, our automated solution performed better than the manual method in a comparison of image quality assessed by board-certified radiologists in future studies.